Prognostic Marker for Acute Myeloid Leukemia (AML) Relapse
Researchers at McMaster University have developed a prognostic method for determining patient survival and prediction of treatment failure in Acute Myeloid Leukemia (AML).
Tech ID
24-095
Inventors
Cameron Hollands
Mick Bhatia
Patent Status
US Provisional Patent Application Filed.
Stage of Research
Proof of principle data available; Cell Reports Medicine, 2024.
Contact
Amy Hector
Business Development Manager
Abstract
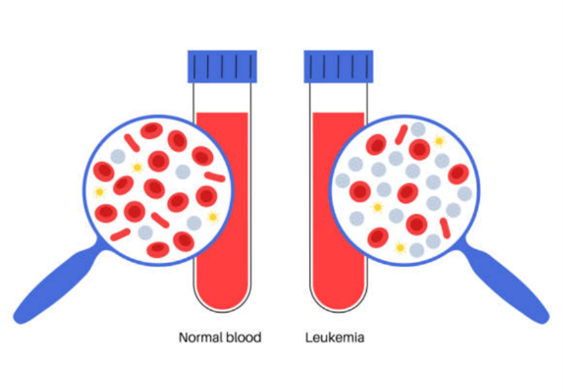
Acute Myeloid Leukemia (AML) is an aggressive and heterogeneous cancer characterized by abnormal differentiation of myeloid blood cells [1]. While considerable advancements in AML treatment have been made, the long-term survival rate of AML is still less than 50% in younger patients and only around 15% for older adults today [2]. A key challenge is that surviving leukemic cells contribute to relapse post-chemotherapy, but little is known about these enduring leukemic cells and how they reinitiate disease, leading to a lack of methods to monitor disease post-intervention and lack of therapies to combat AML relapse.
Researchers from McMaster University have identified a new population of cells defined by CD74/CD68 expression, termed AML regeneration enriched cells (RECs), which play a crucial role in the regeneration of AML following chemotherapy [3]. Based on this discovery, a prognostic method has been developed for prediction of patient survival and treatment failure in AML.
Applications
- Discovery of targets and pathways within the REC population to serve as markers and indicators of AML relapse.
- Diagnostic metrics and tool for AML treatment planning and prognosis.
- Development of targeted therapies aimed at reducing leukemia regeneration via RECs and their associated pathways.
Advantages
- Improved understanding of AML relapse mechanisms.
- Establishment of prognostic markers to predict whether a patient will relapse.
- Help clinicians navigate treatment options and disease management to administer personalized approaches for AML patients.
References
- Khwaja, A., Bjorkholm, M., Gale, R. E., Levine, R. L., Jordan, C. T., Ehninger, G., Bloomfield, C. D., Estey, E., Burnett, A., Cornelissen, J. J., Scheinberg, D. A., Bouscary, D., & Linch, D. C. (2016). Acute myeloid leukaemia. Nature Reviews Disease Primers, 2(1), 1–22. https://doi.org/10.1038/nrdp.2016.10
- Patel, A., Agha, M., Raptis, A., Hou, J.-Z., Farah, R., Redner, R. L., Im, A., Dorritie, K. A., Sehgal, A., Rossetti, J., Saul, M., Normolle, D., Lontos, K., & Boyiadzis, M. (2021). Outcomes of Patients With Acute Myeloid Leukemia Who Relapse After 5 Years of Complete Remission. Oncology Research, 28(7–8), 811–814. https://doi.org/10.3727/096504020X15965357399750
- Hollands, C.G., Boyd, A.L., Zhao, X., Reid, J.C., Henly, C., ElRafie, A., Boylan, D., Broder, E., Kalau, O., Johnson, P., Mark, A., McNicol, J., Xenocostas, A., Berg, T., Foley, R., Trus, M.., Leber, B., Garcia-Horton, A., Campbell, C., Bhatia, M. (2024). Identification of cells of leukemic stem cell origin with non-canonical regenerative properties. Cell Reports Medicine, 101485. https://doi.org/10.1016/j.xcrm.2024.101485
Image obtained from: https://www.istockphoto.com/vector/leukemia-cancer-disease-gm1358654348-432215562?searchscope=image%2Cfilm

